Sharp abdominal twinges after a meal can be alarming, especially when you have no idea what’s causing them. Gallbladder trouble often sneaks up quietly, yet it leaves clues. One of the earliest signs of a gallbladder issue is abdominal pain, typically felt in the upper right side or center of the abdomen. This discomfort is often accompanied by digestive distress after meals, such as bloating or nausea. Many individuals also notice changes in their bowel habits, including diarrhea or unusually light-colored stools. Frequent indigestion, especially after eating fatty foods, can further signal that something may be wrong with the gallbladder.
Key Takeaways
- Upper-right abdominal pain that intensifies after eating—especially rich, fried, or greasy foods—is often the very first alarm bell. Because the sensation can radiate to your back or right shoulder, it’s easy to mistake for muscle strain.
- Persistent bloating, belching, and a heavy, full feeling within minutes of finishing even modest meals suggest sluggish bile flow and early gallbladder dysfunction, especially when relief comes only after avoiding fatty dishes altogether.
- Sudden bouts of nausea or vomiting that appear out of the blue—often in the evening—are common in the early stages of gallbladder disease and differ from food poisoning because there’s rarely fever or widespread stomach cramping.
- Stools that float, look unusually pale, or leave oily residue in the toilet indicate fat is passing through undigested—an unmistakable sign that bile is not being released properly from the gallbladder into the small intestine.
- In Loveland, CO, chilly winter comfort foods paired with an active outdoor lifestyle can make subtle symptoms easy to ignore, but early evaluation by a local digestive health specialist may prevent emergency surgery later.
- Family history of gallstones, rapid weight loss, high-fat diets, and certain medications all raise your risk; catching the first whispers of trouble lets you adjust habits and partner with your provider for prevention.
Gallbladder
How Your Gallbladder Works—and Why It Matters
Your gallbladder sits tucked under the liver, quietly storing and concentrating bile until you eat. Although it’s small, this pear-shaped organ plays a vital role in digesting fats and absorbing fat-soluble nutrients. When its delicate balance is disrupted, the first signs of trouble often appear suddenly—but they’ve usually been brewing beneath the surface for months or even years.
Gallbladder Basics: Storage and Concentration of Bile
Your liver continuously produces bile. Instead of dumping it straight into the intestine, the body parks most of the fluid in the gallbladder, where water is removed so the bile becomes extra potent. That concentrated bile is released in controlled spurts when fatty food reaches your small intestine.
Bile’s Role in Digestion
Bile acts like a detergent, breaking large fat droplets into smaller ones that pancreatic enzymes can finish off. Without enough bile, dietary fats—and the vitamins they carry—slide through the gut undigested. You’ll notice greasy stools, bloating, and lingering fullness.
What Happens When Flow Is Blocked?
Gallstones, bile “sludge,” or inflammation can clog the narrow ducts that empty the gallbladder. Pressure builds, tissues swell, and nerves fire pain signals. Over time, poor bile flow sets the stage for infection (cholecystitis) or even pancreatitis.
Center
Northern Colorado patients have several high-quality center choices when they need gallbladder help. UCHealth Medical Center of the Rockies in Loveland, Banner McKee Medical Center, and North Colorado Medical Center in Greeley all provide advanced imaging, minimally invasive surgery, and integrated after-care. Choosing a digestive health center close to home cuts travel time, speeds early diagnosis, and lets your surgeon coordinate seamlessly with your primary doctor.
Spotting the First Signs: Pain, Digestive Distress, and More
Subtle gallbladder symptoms can masquerade as heartburn, gas, or simple “food not agreeing” with you. Recognizing patterns—especially around meal times—helps distinguish a minor digestive hiccup from early gallbladder dysfunction.
Pain Patterns You Shouldn’t Ignore
The classic gallbladder attack begins as a dull ache in the upper right abdomen, escalating to stabbing pain that can last minutes to hours. It often flares 30–60 minutes after eating fried or creamy dishes. Because the diaphragm shares nerve paths, discomfort may travel to the right shoulder blade or mid-back, making it easy to misdiagnose as a pulled muscle.
Digestive Distress After Meals
Bloating, gassiness, and nausea shortly after mealtime point to sluggish bile flow. Without bile’s emulsifying magic, fats linger in your stomach and small intestine, causing that “brick in the belly” sensation. If you notice relief when skipping fatty foods, your gallbladder may be crying for help.
Changes in Bowel Habits
When bile pigments don’t reach the intestine, stools lose their normal brown color, appearing clay-colored or pale. Floating stools that leave an oily ring suggest malabsorption of fat. Alternating diarrhea and constipation are also common, especially as the gut microbiome reacts to undigested lipids.
Option
Early-stage gallbladder disease rarely demands immediate removal. Your option list usually starts with conservative measures:
- Diet modification to lower saturated fat.
- Prescription ursodeoxycholic acid to dissolve small stones.
- Antispasmodic medication to calm duct spasms.
- Endoscopic approaches like ERCP if a single stone blocks the common bile duct.
If these steps fail or if infection sets in, laparoscopic surgery becomes the superior option—offering quick recovery and minimal scarring. Your surgeon will discuss every option and respect your treatment goals.
Greeley
Residents of Greeley face the same gallbladder risks as Loveland but often commute longer distances for work in agriculture or energy. Skipping meals, then grabbing high-fat fast food on the road, creates the perfect storm for stone formation. Banner Health’s digestive clinic on 16th Street offers walk-in ultrasound scanning so you can get a same-day diagnostic report and avoid a late-night ER visit in severe abdominal pain.
Gallstone
A gallstone forms when cholesterol or pigment particles clump in stagnant bile. Stones range from a grain of sand to golf-ball size. The first thing most patients notice is not the stone itself—it’s the sudden, intense abdominal pain known as biliary colic. If the stone shifts and blocks the duct completely, infection and pancreatitis can set in within hours. Early diagnosis with ultrasound is crucial to treat the condition before complications escalate.
Loveland, CO Factors That Influence Gallbladder Health
Life in Northern Colorado brings unique influences—from altitude to local cuisine—that can sway gallbladder wellness. Understanding these regional factors helps you tweak habits in ways that make sense for your lifestyle.
Comfort Food Meets Outdoor Adventure
Cold winters inspire rich stews, green-chile-smothered burritos, and buttery baked goods. Combine those high-fat favorites with weekend hikes and mountain biking, and you get big fluctuations between heavy calorie loads and intense calorie burn—conditions ripe for gallstone formation.
Altitude, Hydration, and Bile Viscosity
At Loveland’s 4,982-foot elevation, dehydration happens faster. Less fluid in your system equals thicker bile, which can crystallize into stones. Carry a refillable bottle and aim for at least half your body weight in ounces of water daily to keep bile moving.
Local Health Resources
Loveland boasts advanced imaging centers and surgeons experienced in laparoscopic cholecystectomy. Establishing care with a primary provider familiar with local protocols ensures prompt referral if symptoms escalate, reducing wait times should you need an ultrasound or HIDA scan.
How Doctors Diagnose Gallbladder Problems in Northern Colorado
Because early symptoms overlap with heartburn, ulcers, and IBS, accurate diagnosis requires a layered approach. Physicians in Loveland follow evidence-based guidelines to pinpoint gallbladder disease while ruling out other culprits.
Physical Exam and Lab Tests
Your provider will gently press on the right upper quadrant; sharp pain on inhalation (Murphy’s sign) hints at inflammation. Bloodwork checks liver enzymes, bilirubin, and pancreatic markers. Elevated values suggest bile duct obstruction or infection.
Imaging That Tells the Full Story
- Ultrasound: First-line, noninvasive, and highly sensitive for gallstones and gallbladder wall thickening.
- HIDA Scan: Tracks radioactive dye through bile ducts to evaluate gallbladder emptying (ejection fraction).
- CT or MRI: Helpful for complicated cases or when stones lodge higher in the biliary tree.
Functional Tests
If pain persists but imaging is normal, your specialist may order endoscopic ultrasound (EUS) or manometry to detect microlithiasis or sphincter of Oddi dysfunction—conditions that mimic gallbladder disease.
Treatment Paths—from Lifestyle Tweaks to Surgery
The right treatment depends on severity, stone size, and how much the symptoms disrupt daily life. Northern Colorado clinicians prioritize conservative measures first, escalating only when necessary.
Diet Adjustments: Your First Defense
Adopting a Mediterranean-style menu rich in fruits, veggies, lean proteins, and healthy fats (olive oil, avocado) reduces gallbladder stress. Limit fried foods, full-fat dairy, and processed meats. Smaller, more frequent meals prevent the bile “rush hour” that triggers pain.
Medications and Non-Surgical Options
- Ursodeoxycholic acid can dissolve small cholesterol stones over months.
- Antispasmodics ease duct spasms, reducing pain.
- IV antibiotics treat acute infection (cholecystitis) when surgery must wait.
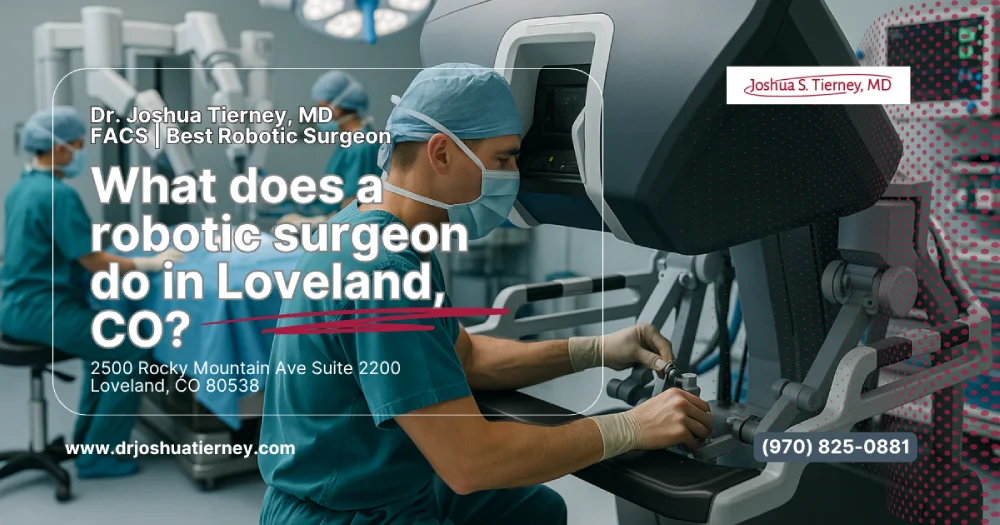
Surgical Interventions
When stones are large, numerous, or causing repeated attacks, laparoscopic cholecystectomy is the gold standard. Loveland hospitals perform this minimally invasive procedure routinely—often as same-day surgery—with quick recovery and small scars. For high-risk patients, endoscopic retrograde cholangiopancreatography (ERCP) may remove duct stones while leaving the gallbladder intact.
Prevention Tips to Keep Your Gallbladder Happy
Even if you haven’t felt a single twinge, protecting your gallbladder makes sense—particularly if risk factors run in your family. Small lifestyle shifts pay big dividends in digestive comfort.
Smart Eating Habits
- Prioritize fiber-rich foods like oats, beans, and leafy greens to keep cholesterol in check.
- Trade saturated fats for omega-3s found in salmon, walnuts, and flax.
- Add turmeric, ginger, and leafy herbs—research suggests they stimulate gentle bile flow.
Exercise & Weight Management
Aim for 150 minutes of moderate aerobic activity each week. Slow, steady weight loss (1–2 pounds per week) prevents the rapid gallstone formation often seen after crash diets or bariatric surgery.
When to Schedule Checkups
- Any unexplained upper-right abdominal pain lasting longer than 15 minutes.
- Nausea or vomiting after fatty meals more than twice a week.
- Pale or greasy stools persisting for three days.
Early evaluation lets your provider order an ultrasound before an emergency lands you in the ER.
The first whispers of gallbladder trouble—upper-right abdominal pain, post-meal bloating, pale stools, and sudden nausea—often appear long before an emergency “attack.” By recognizing these subtle signs, staying hydrated at Loveland’s higher altitude, and adjusting your diet toward leaner, fiber-rich choices, you can protect this small but essential organ. If discomfort persists, prompt imaging and expert guidance from a Northern Colorado digestive specialist can keep minor issues from escalating. Listen to your body, trust your gut (literally), and book a checkup when something feels off—your future self will thank you.
FAQs
What’s the first thing I should do if I feel severe abdominal pain after eating?
Call your doctor or head to an urgent care clinic immediately. Severe abdominal pain that peaks within an hour of a fatty meal is a classic sign of a gallbladder attack. Early diagnosis with ultrasound helps prevent infection or a trip to emergency surgery.
Can reflux and gallbladder disease feel similar?
Yes. Acid reflux causes burning behind the breastbone, while gallbladder pain sits higher under the right ribs. Still, both can involve nausea and chest discomfort. A diagnostic work-up, including imaging, clarifies which condition is behind your symptoms.
How long can I wait before deciding on gallbladder removal?
If attacks are mild and infrequent, lifestyle and medication may control symptoms for months. However, repeated pain episodes, infection, or gallstone migration require prompt surgery. Discuss every option with a specialist to balance risk and quality of life.
Does UCHealth offer non-surgical treatment in Loveland?
UCHealth clinics provide diet counseling, bile-dissolving medications, and endoscopic stone removal. These healthcare services give patients an option to avoid or delay removal surgery when the condition is caught early and stones are small.
Are all gallstones visible on a regular ultrasound?
Most cholesterol stones appear clearly, but tiny “sludge” particles or pigment stones may hide. If your symptoms persist despite a normal scan, your surgeon may order HIDA imaging or endoscopic ultrasound for a more detailed diagnostic report.
How does Banner Health in Greeley manage emergency gallbladder attacks?
Banner’s ER team starts IV fluids, pain control, and blood tests right away. Rapid imaging pinpoints the stone, and an on-call surgeon decides whether immediate laparoscopic removal or ERCP stone extraction is the safest treatment.
Can I still digest fat after my gallbladder is removed?
Yes. Your liver keeps making bile, but it now drips steadily into the intestine rather than being stored. Most patients digest fat normally within weeks, though limiting large, greasy meals early on reduces post-surgery discomfort.
Is early diagnosis really that important?
Absolutely. Detecting gallbladder disease before infection or pancreatitis develops means easier surgery, shorter hospital stays, and fewer long-term health problems. Early diagnosis also offers time to try medical management if you’d prefer to avoid surgery.
What role does diet play once stones have already formed?
A low-fat, high-fiber diet won’t dissolve existing stones, but it minimizes painful contractions and may prevent new stones from forming. Combined with weight regulation, diet remains a cornerstone of conservative gallbladder treatment in Loveland and Greeley.
Can recurrent nausea without pain indicate gallbladder trouble?
Yes. Some patients experience queasiness, loss of appetite, or intolerance to fatty foods long before they feel sharp pain. Persistent nausea, especially if paired with pale stools, warrants a thorough gallbladder evaluation at a trusted medical center.